THE PERICARDIUM
CONTENTS
- How to find the pericardium
- What’s normal?
- Is this a pericardial effusion?
- Is this a tamponade?
- Does size matter?
- 3 cases that really happened to me
- Draining a pericardial effusion
HOW TO FIND THE PERICARDIUM
Any window often suffices, but the liver is such as good sound conductor that the subcostal window usually affords the best view of the pericardium.

WHAT’S NORMAL?
- A small amount of pericardial fluid is normal. It’s there to lubricate the 2 pericardial layers as they slide against each other.
- An anterior fat pad is also ‘normal’ in the obese. Fat pads are fairly echo-poor (dark), so they can mimic pericardial fluid.
IS THIS A PERICARDIAL EFFUSION?
FALSE POSITIVES
- Pericardial fat pad (effusion is usually darker and present in more than one view, often all around the heart)
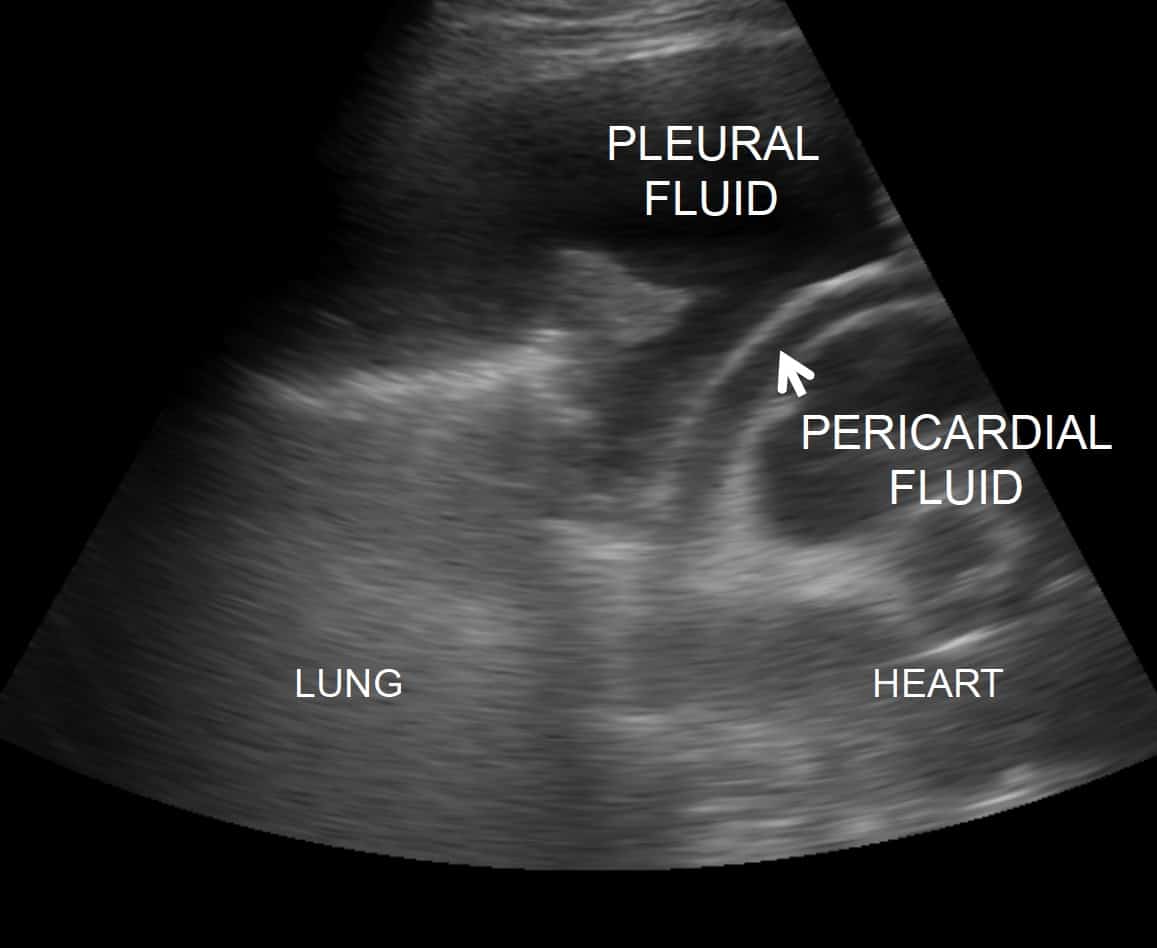
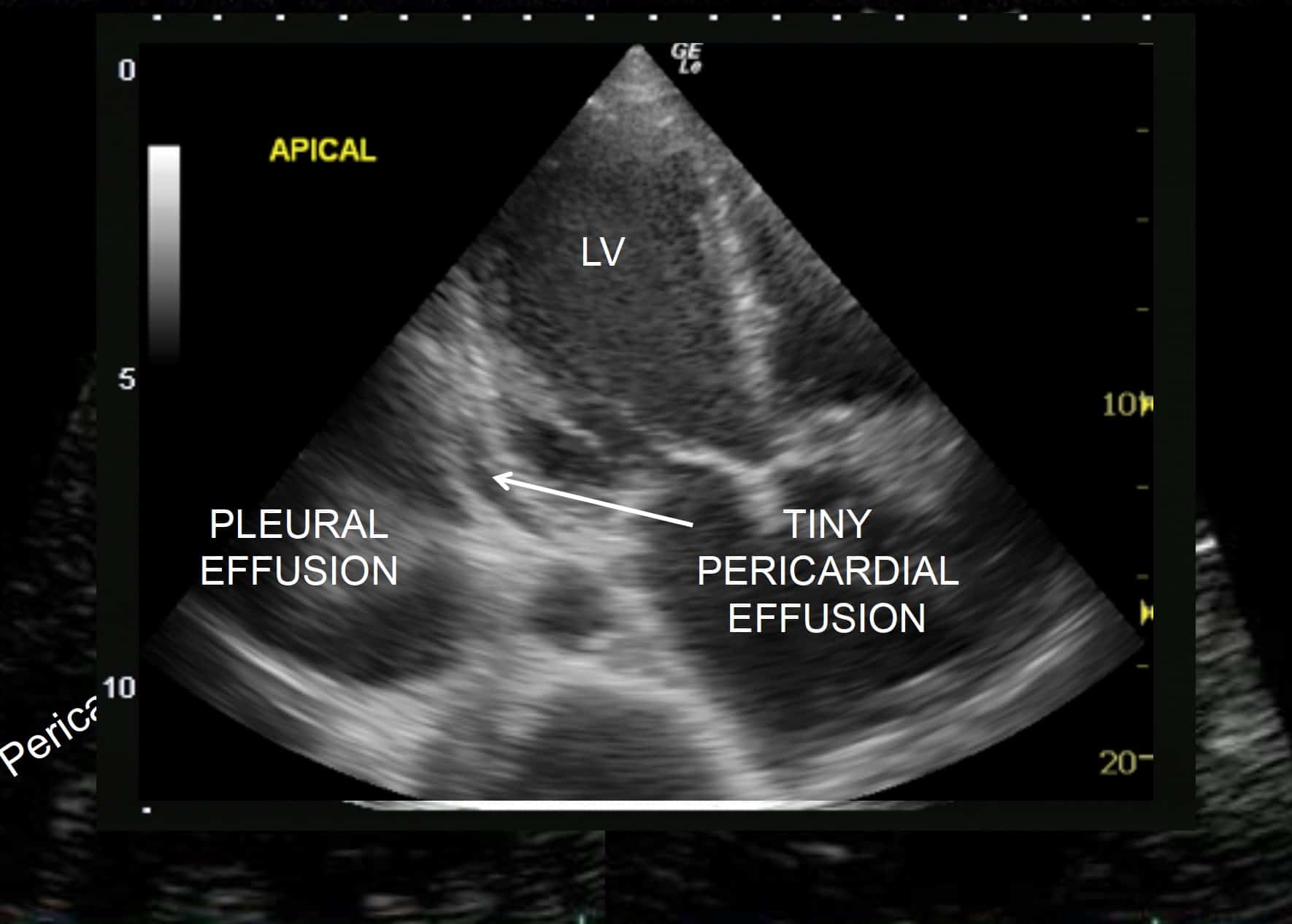
- Pleural effusion: on cardiac views, a left pleural effusion can mimic a pericardial effusion. However, a quick look at the lung base from the lateral side will quickly tell you if a pleural effusion is present. Another tip is that fluid in the pleural space will surround the descending aorta, but fluid in the pericardial space runs in front of the aorta.
FALSE NEGATIVES
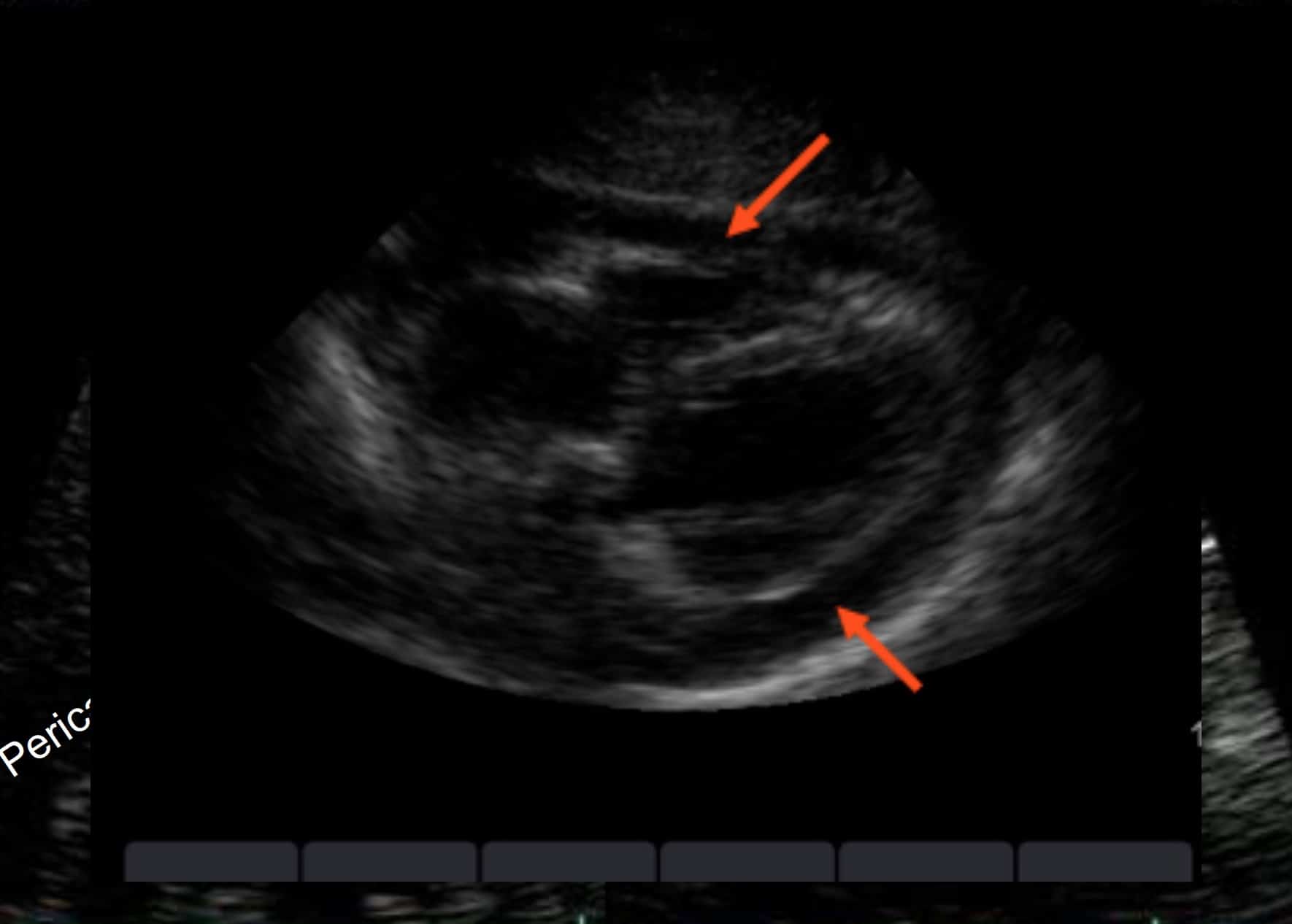
- Clotted blood: critical care clinicians tend to expect that fluid (including blood) is dark on US. However, clotted blood will be echogenic and may resemble liver or be even brighter.
- Heterogenous pericardial collections: clotted blood mixed with fresh blood, proteinaceous strands in malignant / infective effusions
- Loculated pericardial effusion: particularly in the case of recent cardiac surgery, a patient may tamponade due to a small pericardial effusion located over one chamber e.g. the right atrium. These are easily missed by basic echo, and can be very difficult to drain as well.
IS THIS A TAMPONADE?
Tamponade is a clinical diagnosis: i.e. the patient must actually be shocked. If the patient isn’t shocked, you have time to arrange a formal study and chat to your friendly cardiologist.
The 5 features of cardiac tamponade:
1. A shocked patient
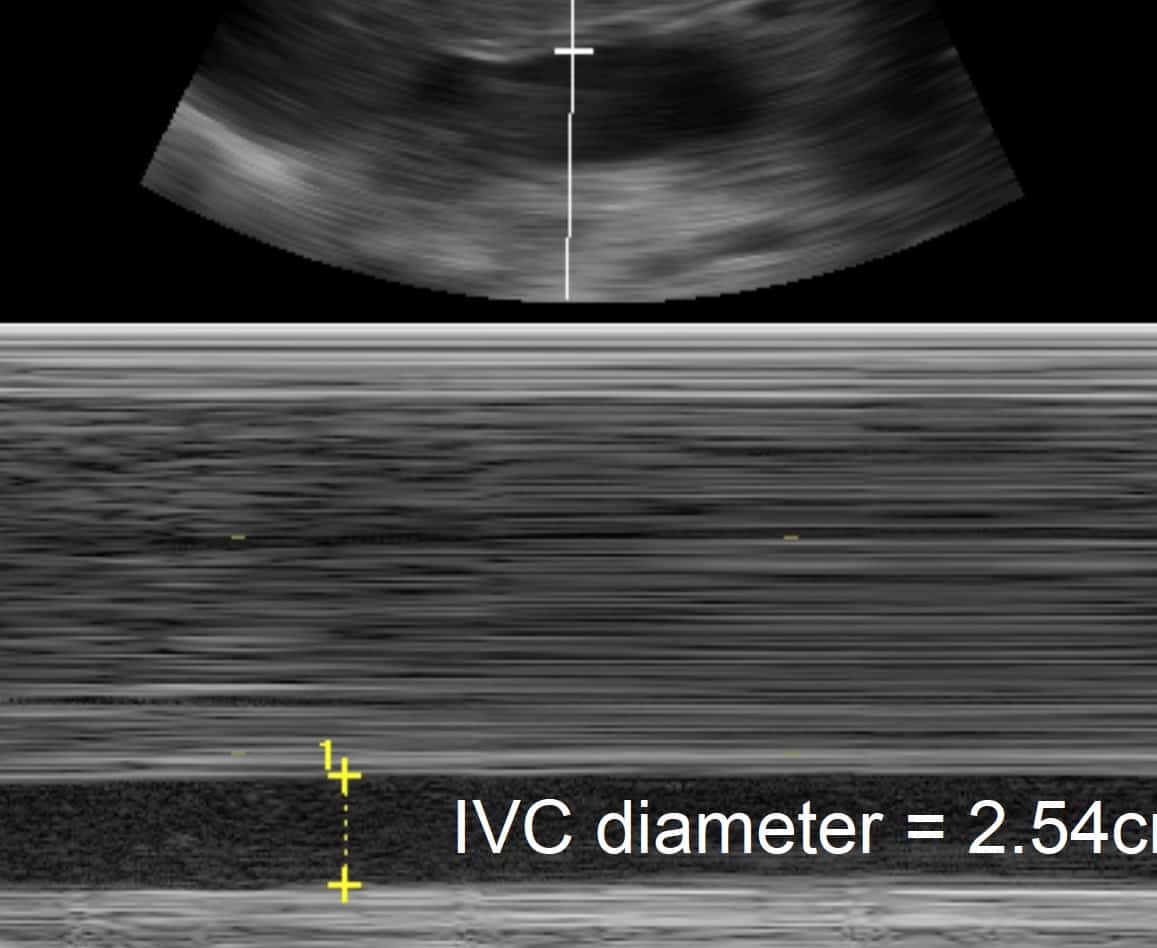
2. Distended veins on US: look for the IVC:
- Dilated
- No respiratory variation
- Very hard to ‘squash’ with the US probe
- If you can’t find the IVC, check the other veins e.g. IJV / EJV. In tamponade, they are dilated as well.
3. ‘Stuff’ in the pericardium on US
- Ideally this will be uniformly dark (echo-poor), but it can be bright or heterogenous. (If there is no pericardial fluid at all, think: has this patient had recent cardiac surgery? Could it be a loculated effusion?)
4. Diastolic collapse of the RA/RV on US
- Although these are the ‘classic US features’ of pericardial tamponade, they can be very hard to see at times.
- Basically, in a tamponade the pressure builds up in the pericardium and this pressure tends to ‘squash’ the cardiac chambers.
- The lowest-pressure chamber is the right atrium (RA) in atrial diastole: when the RA ‘opens up’ to receive blood from the venae cavae, its pressure falls below that of the pericardial space, and the pericardial fluid squashes it.
- As the pressure continues to rise, the same thing happens to the RV.
- BUT things are moving so fast (the patient is in extremis, the heart is beating like the clappers) that this can be bloody hard to see using realtime US.
- Look instead for the RA/RV ‘acting weird’ in their respective diastoles.
- And sometimes it’s easy: the RV is completely squashed by the pericardial fluid.
5. Finally, the size of the effusion
- This is the least important feature of tamponade (see note below).
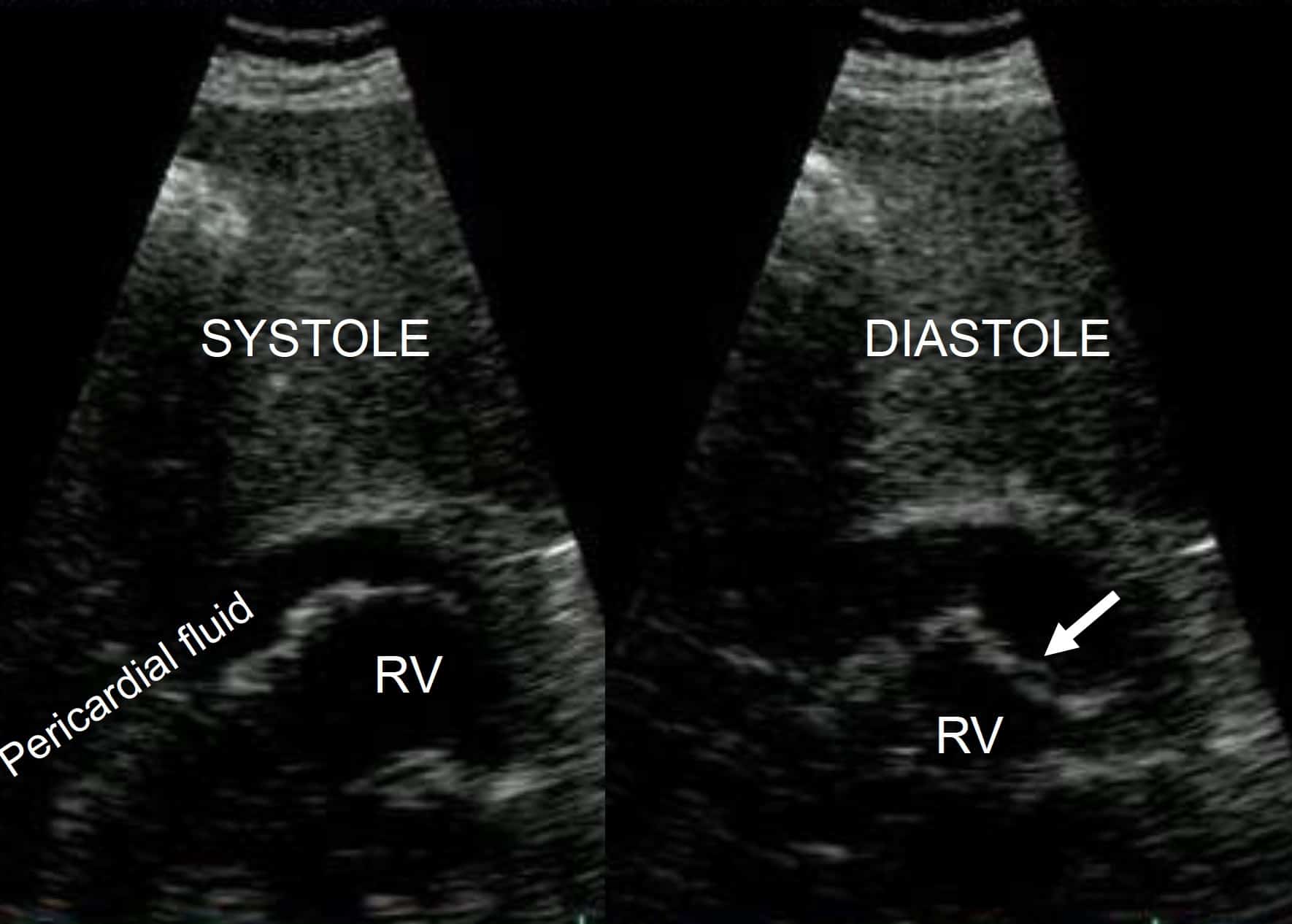
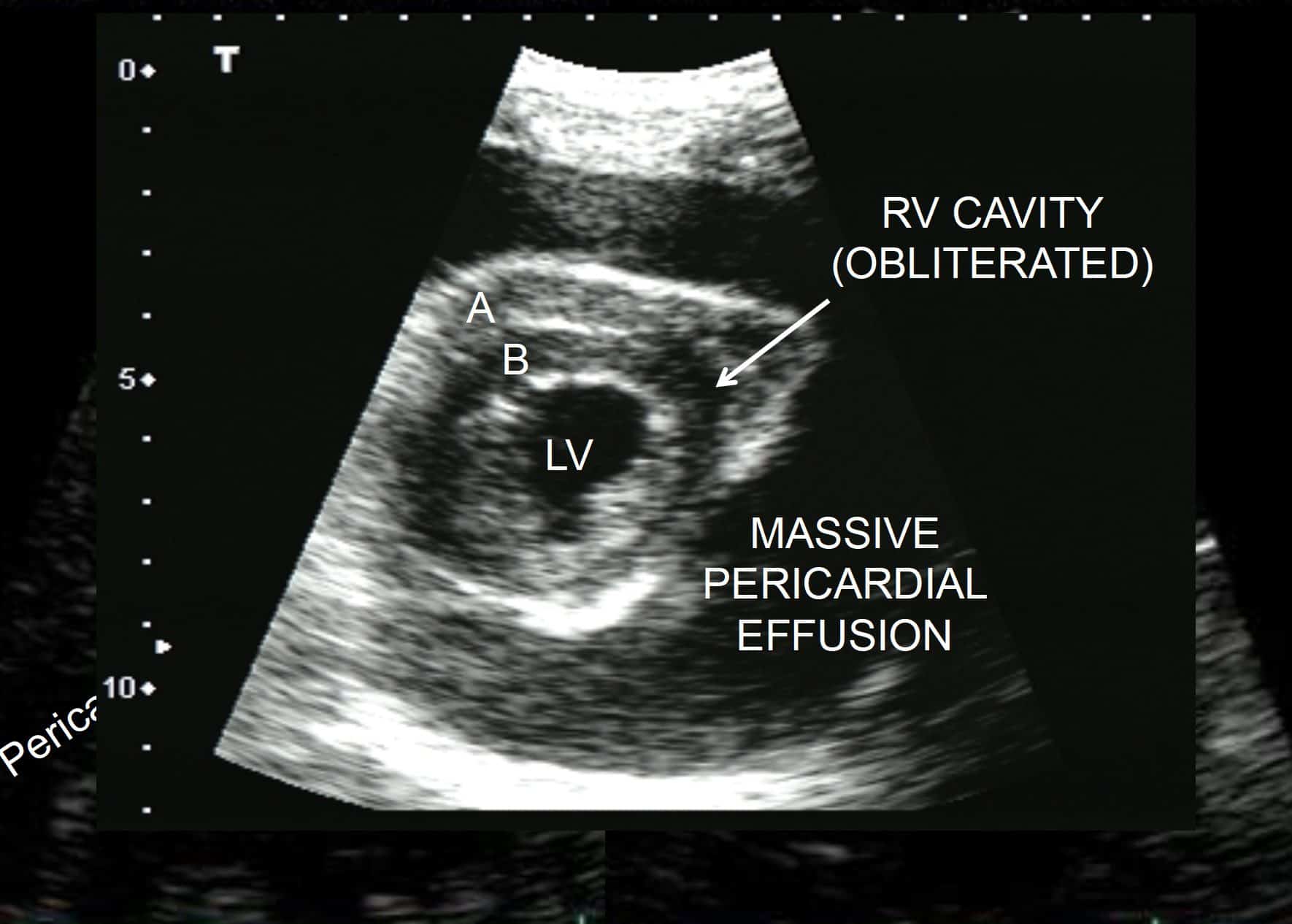
RV cavity is completely obliterated by the high pressures of the pericardial space. Note that this is chronic: the RV free wall (A) is as thick as the IV septum (B).
DOES SIZE MATTER?
Well, when it comes to tamponade: yes and no.
- There is no ‘magic size’ at which a pericardial effusion becomes a tamponade. That’s because the fibrous pericardial sac is a little stretchable, and if a pericardial effusion builds up over time, then the sac can gradually accommodate it (to a point).
- Instead, think of the relationship as a product of volume and time:
- A rapidly increasing effusion (e.g. stabbed RV) will tamponade at low volumes
- A slowly increasing effusion (e.g. uraemic effusion) will tamponade at greater volumes.
- This is why size is much less important than the other four signs described above.
But, everyone still likes to quantify pericardial effusions. So here’s a rough guide:
- Effusion present only in systole (i.e. when the heart chambers ‘pull away’ from the pericardium as they contract)
→ Insignificant. If a low pressure chamber like the RV can ‘chase away’ the fluid in diastole, it’s irrelevant.
- Effusion present throughout the cardiac cycle but not surrounding the heart.
→ In most cases, insignificant for now. (Rarely, loculated effusions cause trouble: see note above.)
- Effusion surrounding the heart.
→ Now you’re talking. Better check the blood pressure and the IVC.
- Effusion so big that heart is ‘rocking’ within it.
→ Any fool can tell you this is important. It’s the reason that ECG in a massive effusion shows ‘electrical alternans’: basically, the heart’s whole axis is changing as it ‘swings’ inside the massive effusion.
ANECDOTE-BASED-MEDICINE
- 3 cases that really happened to JB.
CASE 1.
A retired doctor (well, it would be, wouldn’t it?) turned up to my ED late at night with chest pain, mild breathlessness and recent viral illness. As part of my workup, the US revealed:
- A 2cm pericardial effusion
- RA & RV diastolic collapse
- An IVC of 3cm, with just a little respiratory variation.
But his BP was 120/60, RR 20, sats 100% on 2 litres nasal prong, and the cardiologist elected to wait until the next morning. And he happily survived in the Coronary Care Unit until his effusion was drained the next morning.
CASE 2.
An old woman turned up to the ED shocked and very breathless. She had a known malignant pericardial effusion being managed palliatively.
Predictably, my US showed a very large pericardial effusion, but it also showed a slit-like, collapsing IVC.
Turned out she had septic shock as the cause of her presentation, and she lived to fight another day after judicious IV fluids and antibiotics.
CASE 3.
A middle aged woman arrived peri-arrest. My bedside US did not reveal an obvious pericardial effusion, but she had a dilated IVC and a squashed RV.
After stabilization, a CT showed pericardial clotted blood that in retrospect was isodense with the liver on US, due to a type A dissection.
DRAINING A PERICARDIAL EFFUSION USING US
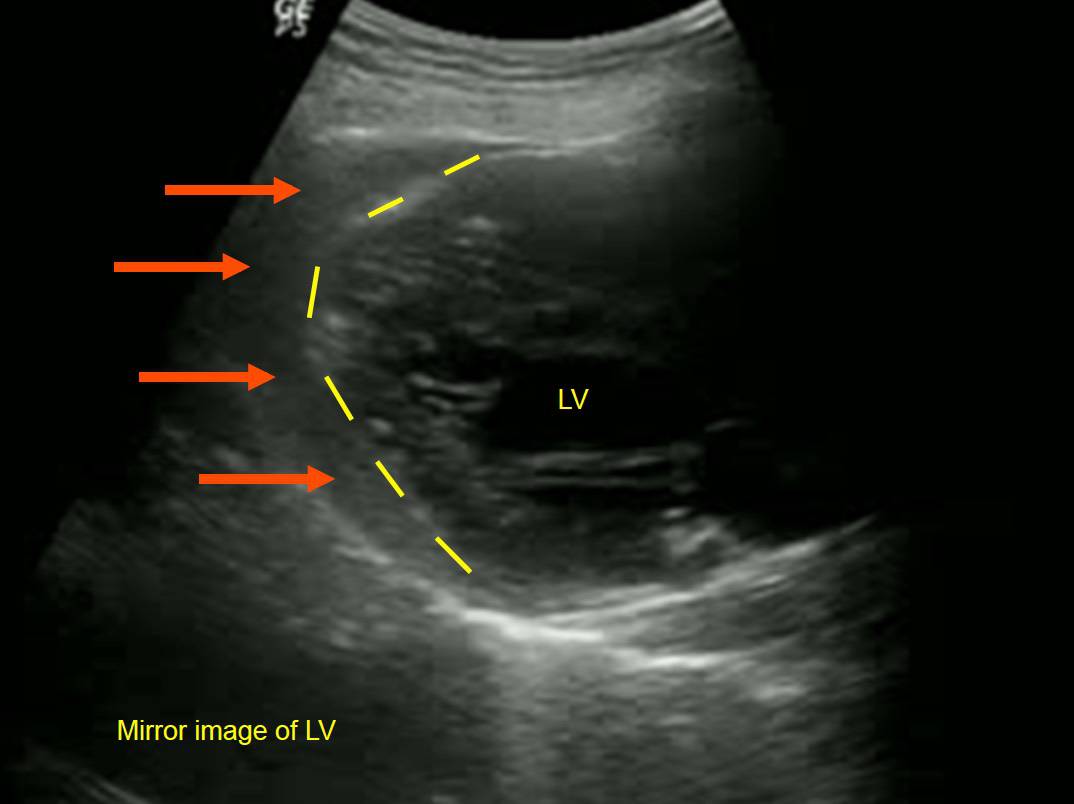
In the pre-US era (‘the old days’), traditionally we were all taught to drain tamponade in the ED via a subcostal approach so as to avoid the lungs. The problem is that this inevitably involves a long needle slicing through the liver.
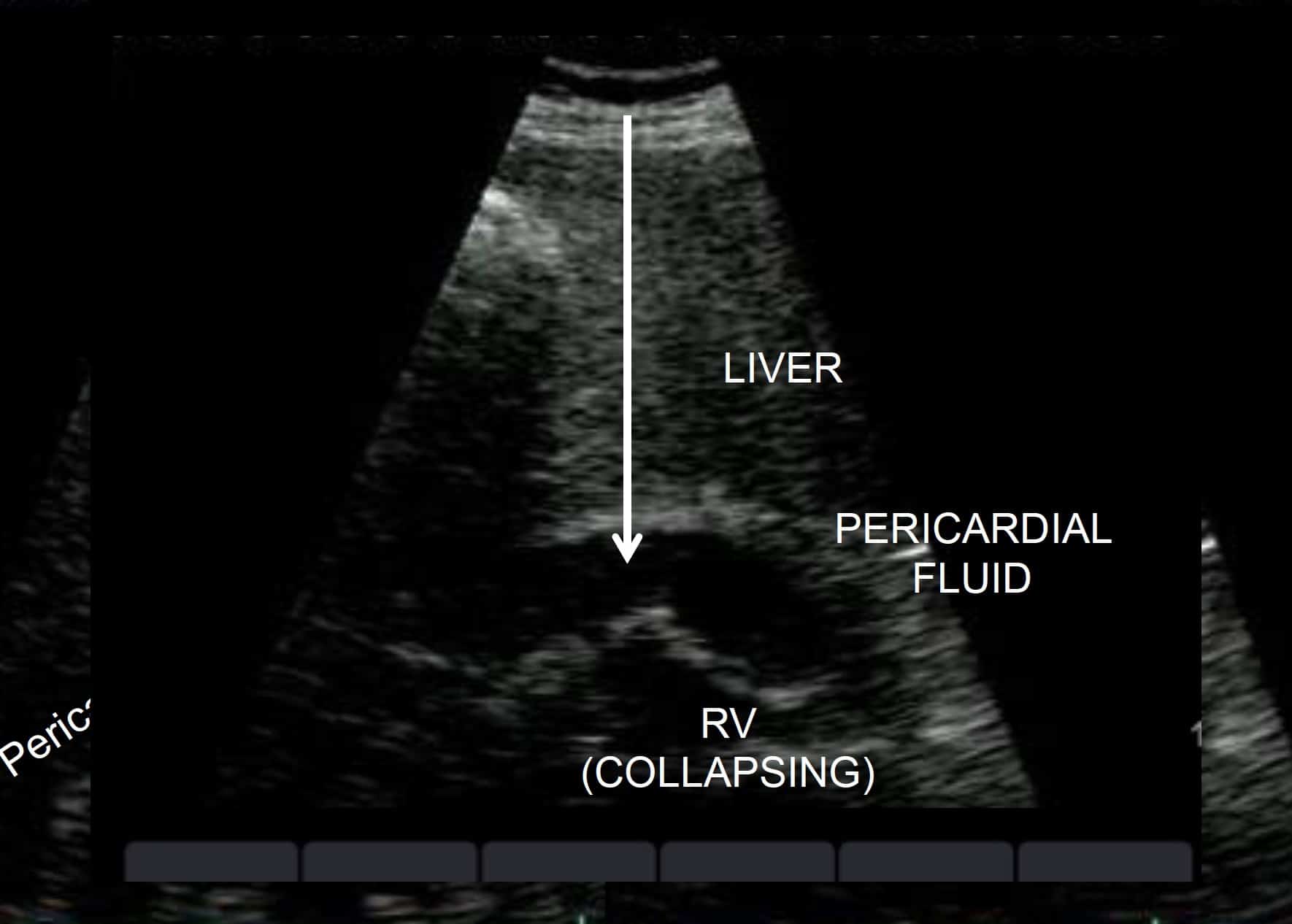
Tamponade, subcostal view. Arrow through liver indicates the direction of the needle using the traditionally taught ‘blind’ pericardiocentesis technique.
THE ADVANTAGES OF US GUIDANCE ARE THAT:
- You can see what you’re doing, so you’re less likely to prang the heart
- You can insert your needle wherever the effusion is greatest and/or closest to the chest wall. In practice, you can needle the heart through the anterior thorax, and even avoid the lungs (because in the left lateral position, a large effusion will push the left lung out of the way).
INDICATION
- Pericardial tamponade
CONTRAINDICATION:
If the pericardiocentesis won’t help, e.g.
- Tamponade due to type A aortic dissection: this patient needs OT. Draining the tamponade with a needle will most likely just lead to reaccumulation. (If the patient is arrested, you might try it.)
- Tamponade due to penetrating trauma: this patient needs a thoracotomy, either in ED or OT.
PREPARATION
TEAM
- Most experienced US proceduralist available, on the patient’s left
EQUIPMENT
- Sterile technique if time permits
- Pericardiocentesis equipment as usual
- It’s nice to attach a 5 or 10ml syringe filled with saline to the end of your needle (why? See below)
- US machine in line of sight, ideally on the right of the patient, facing the operator
PATIENT
- Left lateral if possible (pushes the lung out of the way)
- Ongoing resuscitation by the rest of your team
- Consent? As usual, in an emergency this is implied.
STEPS
1. With non-sterile cardiac probe, choose the best spot to insert your needle (effusion closest to skin surface / largest; see note above). Either mark the skin, or proceed to sterile real-time technique
2. Choose your probe:
a. The cardiac probe will demonstrate the relevant anatomy but often won’t let you see the needle as you insert it (the needle’s angle is too steep and the US frequency is too low).
b. The linear probe will demonstrate the needle (and the effusion, if it abuts the skin) but not the relevant anatomy.
3. Sterilize probe, patient & yourself as you would for any US-guided procedure.
4. Attach the saline-filled syringe to the pericardiocentesis needle and insert it into what you hope is the pericardial space.
5. Then squirt in a small amount of sterile saline: the turbulence & microbubbles will ‘light up’ on screen
a. If pericardial space ‘lights up’, you’re in!
b. If RV lights up, pull out!
6. Complete the pericardiocentesis as usual
























