Having survived to discharge from the ICU, catastrophe strikes our unfortunate 77 year old on the surgical ward with a fall and an acute subdural haematoma. Case 10 of this series asks for your opinion on the appropriateness of ongoing management as well as the optimal management of traumatic intracranial hypertension.
A 77 year old man has been discharged from the ICU to the surgical ward having presented with faecal peritonitis. His ICU stay was complicated by septic shock, ARDS, mild DIC, acute hepatic necrosis and a degree of ICU-acquired weakness.
The patients medical history includes hypertension and hypercholesterolemia, previous heavy alcohol intake, and mild cognitive impairment.
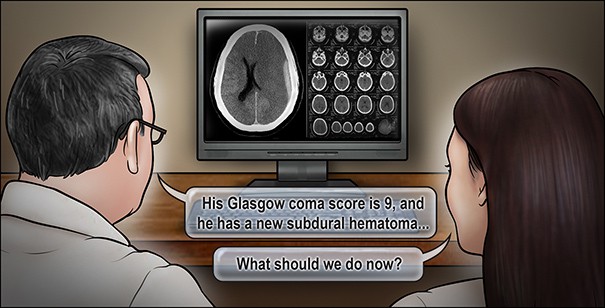
After 15 days in the ICU, the patient is transferred to the surgical floor. On the third morning after discharge from the ICU, he is found on the floor of his room, having apparently fallen from his bed. On examination, he opens his eyes but is not able to speak coherently. He has decreased movement on the right side. His pupils are both midsized and reactive to light. Cranial computed tomography (CT) reveals an acute subdural haematoma in the left hemisphere with underlying hemorrhagic contusion and 5-mm displacement of the midline intracranial structures.
What is the most appropriate management of this patient’s traumatic brain injury?
1. Conservative management, since there is no prospect for functional recovery.
2. Evacuation of the acute subdural haematoma, placement of an external ventricular drain, and admission to the ICU for active management of increased intracranial pressure.
3. Evacuation of the acute subdural haematoma and admission to the ICU for management without monitoring of intracranial pressure.
Cast your vote here and participate in the discussion.
We’ll bring you the poll results and accompanying review when they’re published at the end of the month.