
By Dimity McCracken
These are images from real ICU patients.
[su_tabs][su_tab title=”History”]
76yo man who was initially admitted to ICU with infective exacerbation of COPD. He had been very difficult to wean from ventilatory support. After a fortnight he developed a ventilator-associated pneumonia, & ventilation deteriorated significantly, requiring high pressures. On evening ICU round he suddenly deteriorated: desaturated, poor tidal volumes, & hypotension. What has happened? Why? What would you do next?
[/su_tab][su_tab title=”Image”]
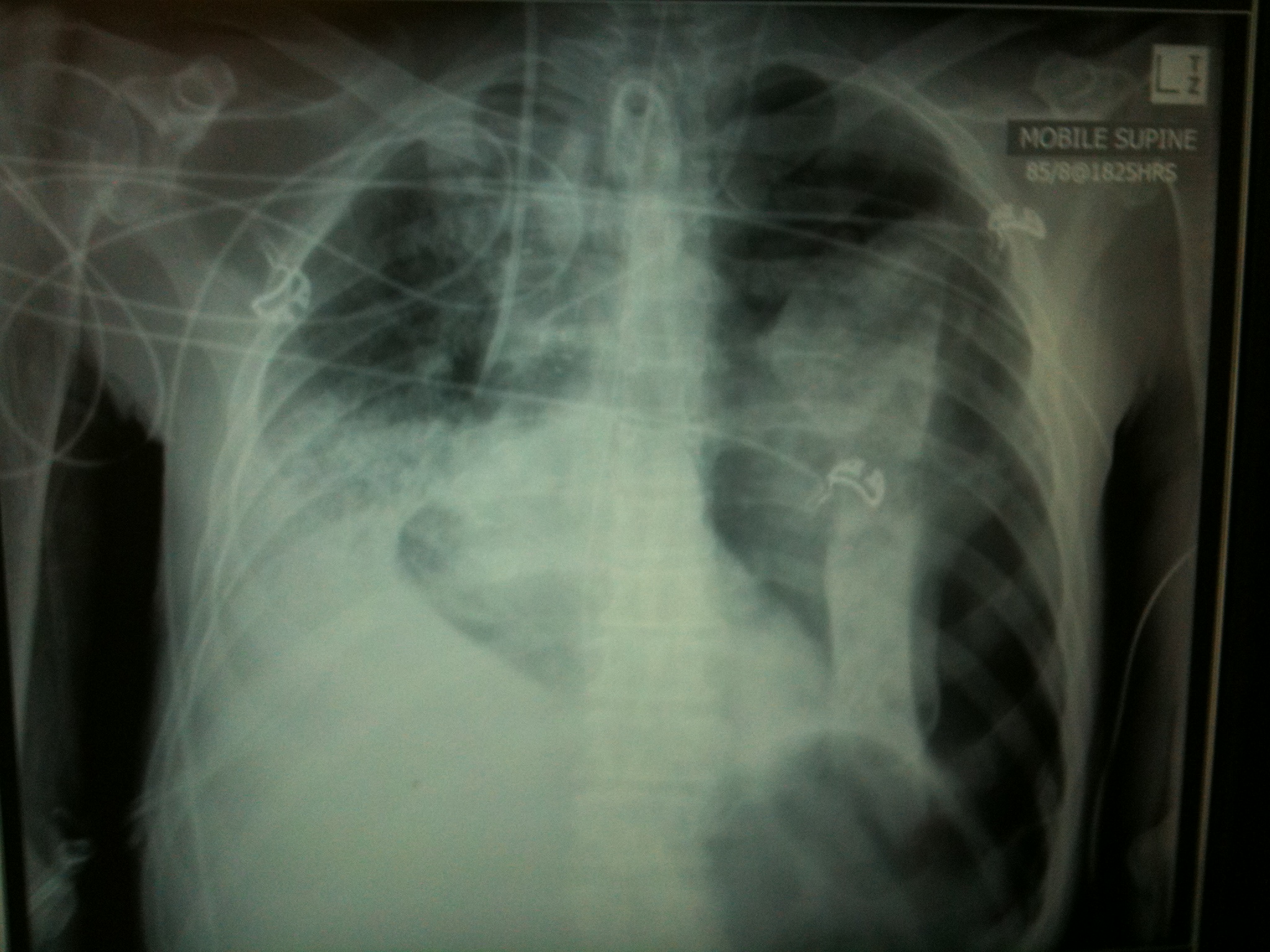
It’s a left tension pneumothorax due to barotrauma, in the setting of severe bullous emphysema. Note patient has a tracheostomy in situ (evidence of long difficult ventilatory wean), R IJ vascath (probable multi-organ failure), L IJ CVC, & significant R lower & mid-zone collapse/consolidation.
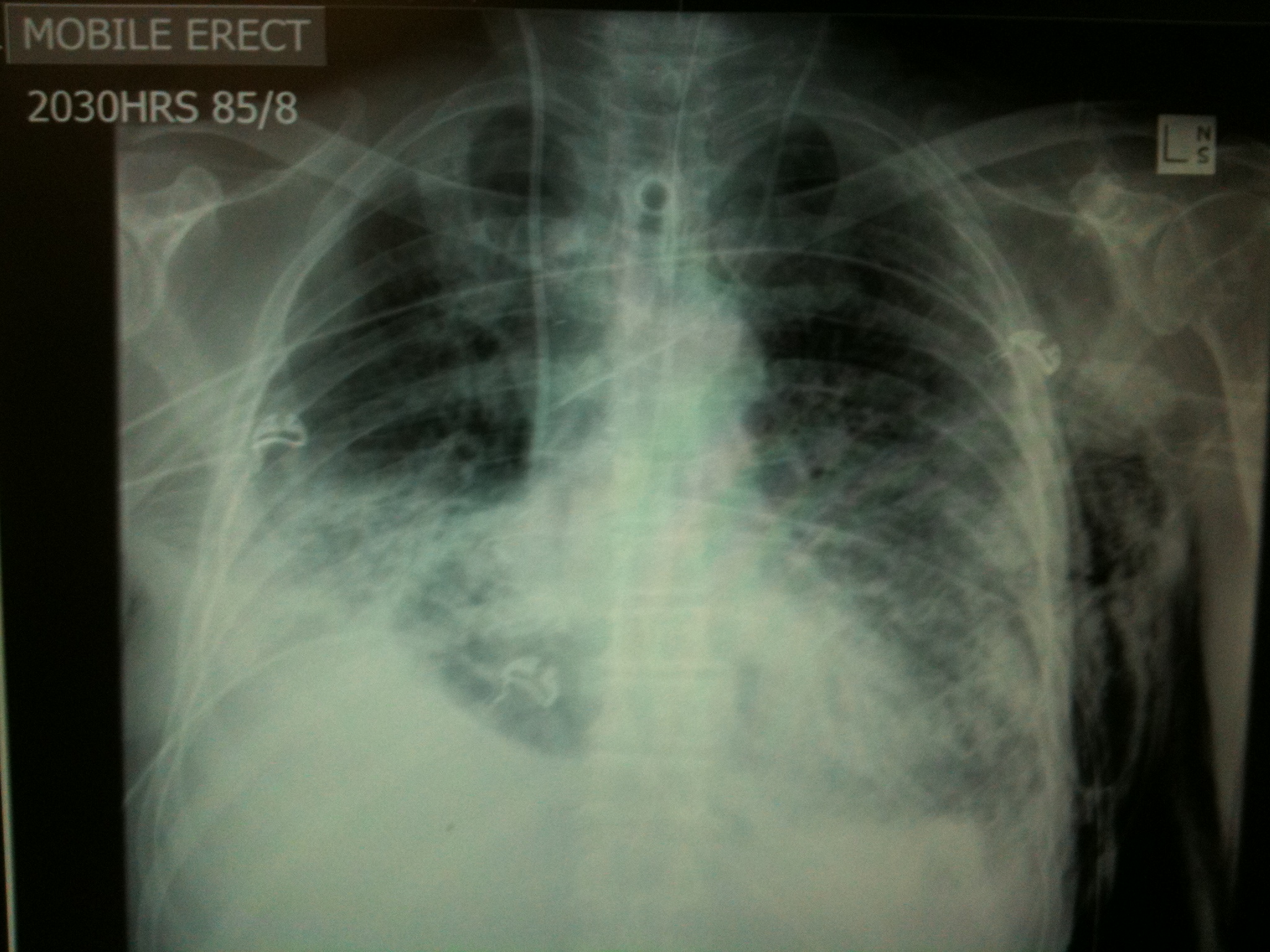
The next step would be to decompress the tension pneumothorax emergently & place an intercostal catheter. Note the significant subcutaneous emphysema, small residual L pneumothorax (may potentially benefit from a 2nd ICC), & bilateral lower & mid-zone collapse/consolidation.
[/su_tab][su_tab title=”More Resources”]
Protective Lung Ventilation evidence on ventilatory strategies from LITFL
Management of COPD from LITFL which includes ventilatory strategies.
High airway pressures: why they occur & how to manage then (again from our friends at LITFL)
Medscape review of Barotrauma – very detailed!
[/su_tab]
[/su_tabs]
























