
By Dimity McCracken
These are images from real ICU patients. The stories and details are changed to preserve confidentiality.
[su_tabs][su_tab title=”History”]
This patient has just returned from cardiothoracic OT. He is ventilated & haemodynamically stable. The nurses mention that the right chest drain is clamped, & ask you if the chest drain should be placed on suction. How do you answer?
[/su_tab][su_tab title=”Image”]
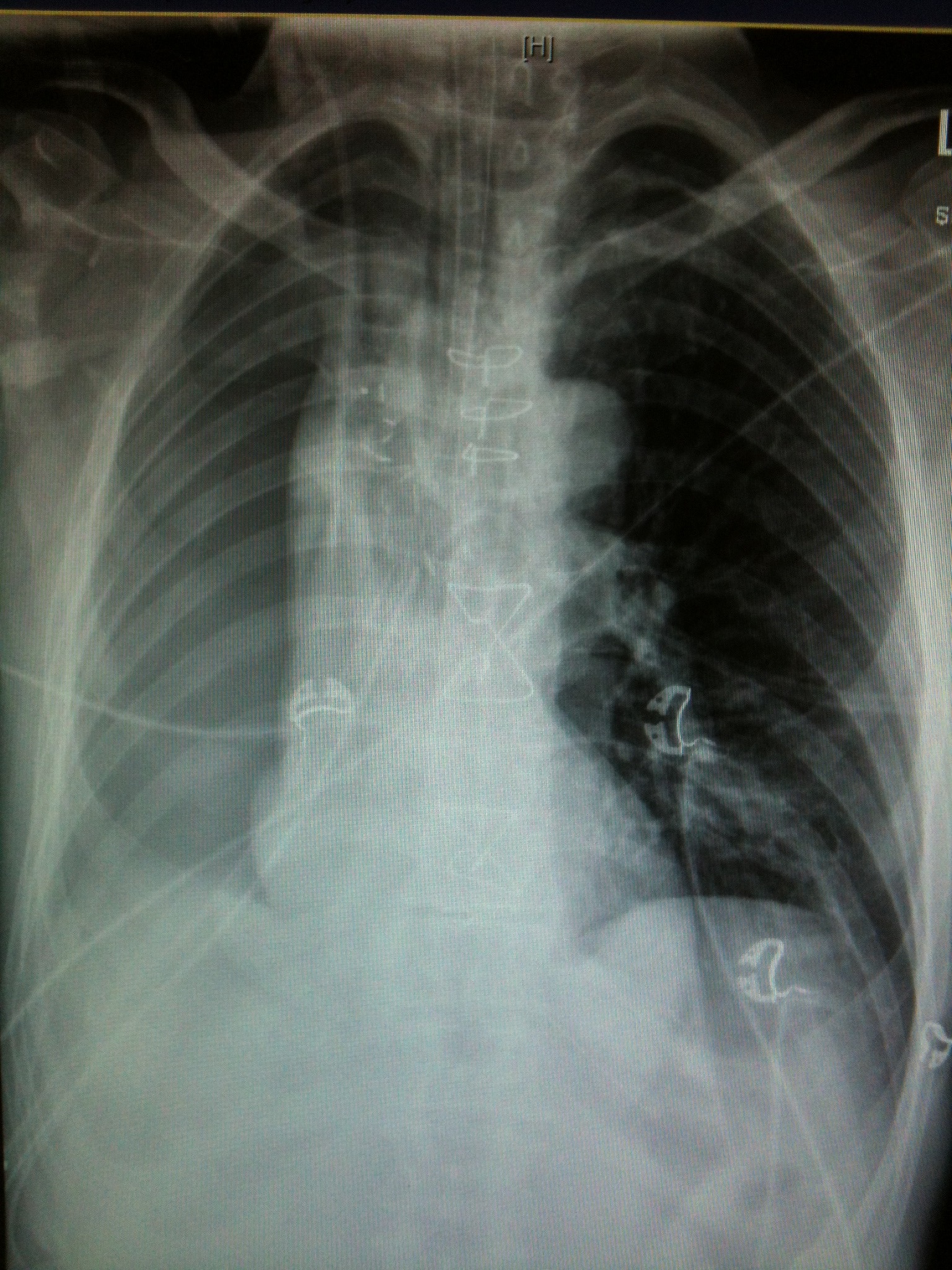
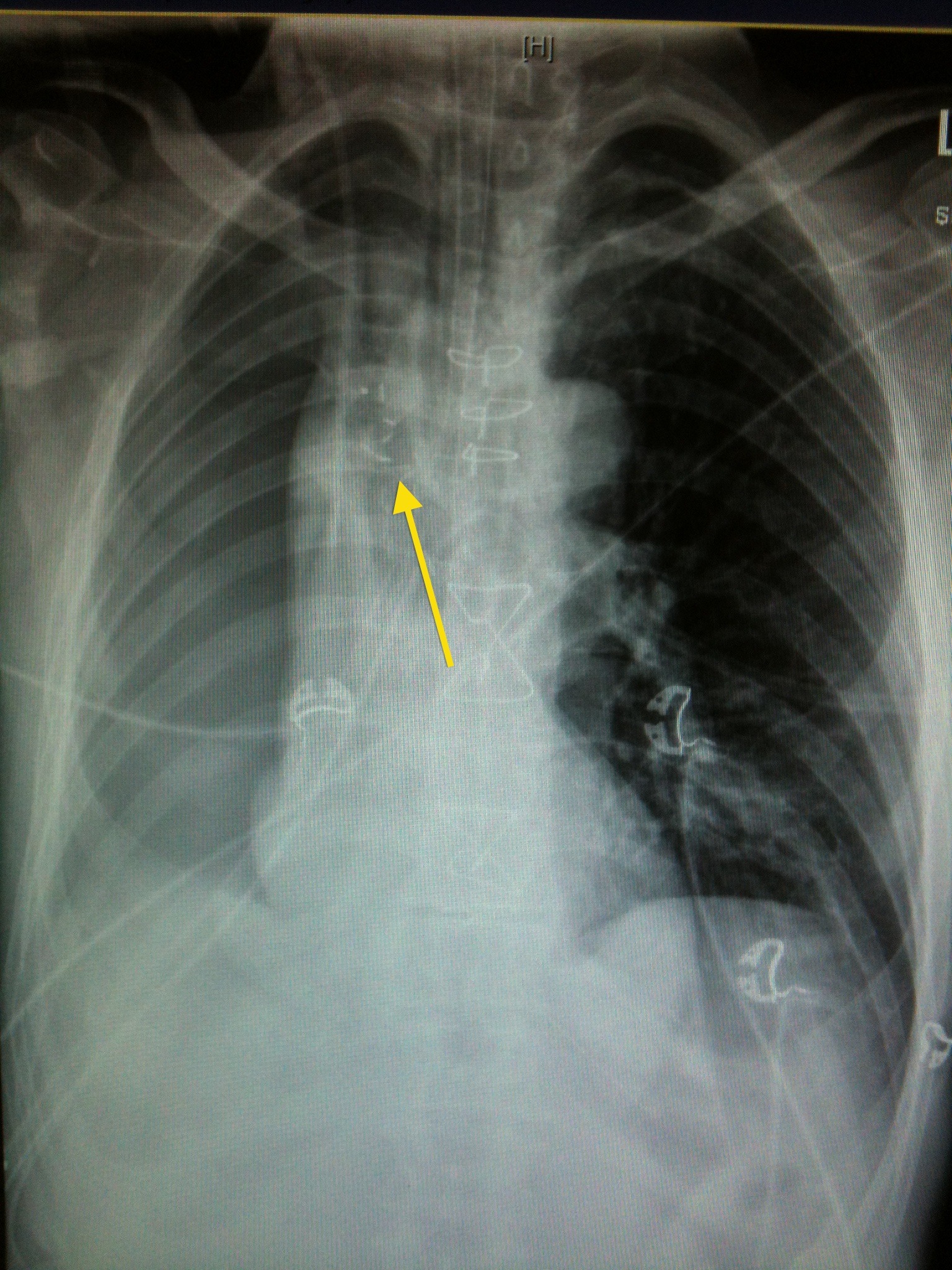
The patient has had a right pneumonectomy. Tell the nurse to leave the chest drain clamped.
The arrow shows the surgical clips over the R bronchial stump. The pneumonectomy looks like a poorly defined but massive pneumothorax. No lung edge is discernable. There is mediastinal shift TOWARDS the right side (the opposite of what one would find if this was a tension pneumothorax). The patient is intubated. There is a right IJ CVC & right ICC visible. Nasogastric tube is appropriately positioned with tip below the diaphragm. Sternal wires are seen (although most pneumonectomies are approached via a thoracotomy). There is some mild L basal atelectasis.
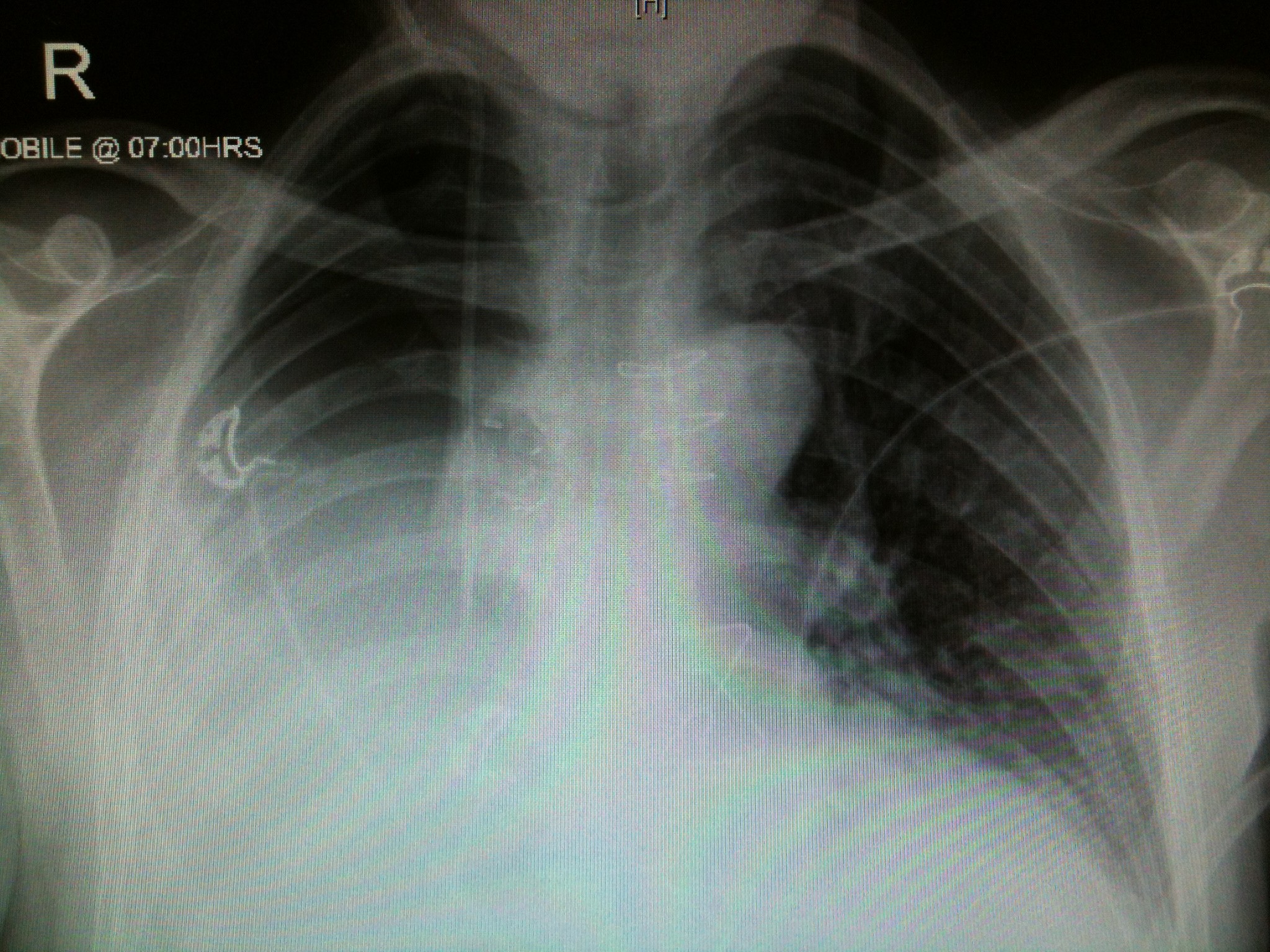
This is their CXR 2days later, once the patient has been extubated & chest drain removed. There has been gradual accumulation of pleural fluid.
[/su_tab][su_tab title=”Management & Resources”]
Management of post-op pneumonectomy patients:
-Ventilation is low pressure ventilation to avoid blasting clips off the bronical stump clips. In addition the pleural pressure is more negative post-op. Thus the remaining lung is hyper-expanded with decreased compliance.
-Do NOT put chest drain on suction! Often leave ICC clamped with intermittent brief unclamping to help regulate pressure on the surgical side, & also to check for post-op haemorrhage. If the ICC is placed on suction it will remove all the air from the surgical side ? no lung available to re-expand that side ? sucks mediastinum across, which then kinks the great vessels ? haemodynamic collapse (similar to tension pneumothorax, except this mediastinal movement is towards the surgical side).
-Post-op haemorrhage can be torrential, so needs to be carefully monitored. Have a very low threshold for a repeat CXR.
-Fluids: keep the patient dry! Immediately post-op these patients are extremely prone to developing pulmonary oedema. Pre-op both lungs received the cardiac output, while post-op this whole output goes through the only remaining lung. This makes the lung very sensitive to any excess fluid & prone to injury (ALI) in addition to the significant reduction in pulmonary reserve.
-Evans article on conservative fluids in lung resection
-Pleural effusion fluid should gradually accumulate over a few days, as air is resorbed. By about 2wks the effusion is clearly visible on CXR: no meniscus sign!
-Very aggressive pulmonary toilet is needed: chest physio, early mobilisation, aggressive management of secretions (including bronchoscopy if required). Due to the acute reduction in pulmonary reserve, these patients do not tolerate any sort of lung insult.
[/su_tab]
[/su_tabs]
























