In the 5th instalment of the NEJM’s case series we were asked to consider the management of an acute disturbance of liver function tests in a 77 year old with severe sepsis who has a background of alcoholism and is on regular paracetamol.
The poll has since closed and the series editors have reviewed the evidence regarding management of multifactorial acute liver failure in a complex ICU patient.
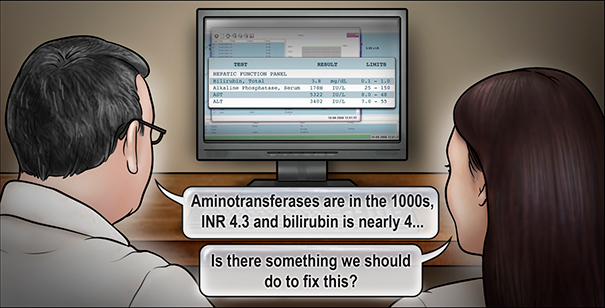
A 77-year-old man has been admitted to the ICU with severe septic shock from fecal peritonitis due to a perforated sigmoid colon. He has a background which includes alcohol abuse and cognitive impairment. Having survived severe septic shock and ARDS his condition has stabilised when suddenly his LFTs become deranged with
- ALT increases to 3402 U/L,
- AST to 5322 U/L,
- Bilirubin to 65 µmol/L.
- INR to 4.3.
His postoperative analgesia includes 1 g IV paracetamol (acetaminophen) every 6 hours.
“What strategy would you use to treat this patient’s acute liver failure?”
The majority of respondents elected to cease paracetamol with 66% commencing acetylcysteine in addition to ongoing supportive care. Only 5% of respondents elected to continue paracetamol at its current or a reduced dose.
The series editors supported the cessation of paracetamol and commencement of NAC to provide increased in oxygen delivery to the necrotic liver. Even in the absence of firm evidence of paracetamol overdose, NAC is appropriate given the minimal risk associated with it. Indeed, the included review article refers to a 2009 RCT demonstrating improved survival with administration of NAC in non-acetaminophen overdose related acute liver failure.
Alternative aetiologies should be considered and excluded with specific investigation which in this case includes ischaemic hepatitis from reduced cardiac output, right heart failure related venous congestion or increased abdominal pressures, drug induced hepatitis, or hepatic vascular occlusion.
The editor’s full response can be found here .

























