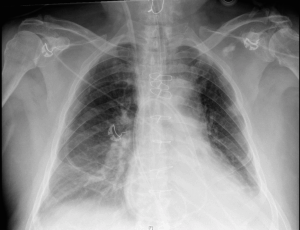
Question:
What do you think about the position of this PA catheter?
Would you trust the readings from it?
[az_toggle_section] [toggle title=”Answer” id=”tgl-1″]This PAC had become knotted in the right ventricle. On the monitor, there was a good PA trace with PA pressures that were expected for the patient. However, their CI had decreased and the PAC was inserted to 75cm. The CXR demonstrated that the PAC had become looped in the RV before entering the PA. The PAC was removed and replaced with a new line.[/toggle] [/az_toggle_section]
The Pulmonary Artery Catheter (PAC), also known as the Swan Ganz Catheter or “The Yellow Snake” was first developed in 1970 by Jeremy Swan and William Ganz. It was developed as a means of enabling pressure monitoring to be accessible in the intensive care unit. Over the years, it has acquired a number of different uses including continuous CO monitoring, central temperature monitoring, measurement of PA pressures (and RA/RV pressures), measurement of mixed venous saturations, atrial and ventricular pacing and estimation of LVEDP.
Although the use of PAC is controversial amongst intensivists, it is considered the gold standard for monitoring CO. They are particularly useful post cardiac surgery but are also commonly used in a number of different settings including myocardial infarction, right ventricular failure, pulmonary hypertension and cardiogenic shock.
The PAC
The PAC is a balloon tipped, quad lumen catheter which is inserted through a sheath. It has 10cm markings along its length the aid insertion. The four lumens include: (1) a proximal injectate port for RA/CVP monitoring and injection of injectate for CO monitoring; (2) a proximal infusion port for drug and fluid infusion; (3) a distal pulmonary artery lumen for PA pressure monitoring and mixed venous SO2; (4) a thermistor for monitoring CO using thermodilation technique.
Insertion
- Identify a suitable large vein, usually the right internal jugular vein, although the left subclavian or femoral veins may be used.
- The introducer sheath is inserted using the Saldinger Technique (usually under ultrasound guidance)
- The PAC is inserted through the sheath and the transducer is used to demonstrate the location of the tip. Once in the RA (approximately 10cm), the balloon is inflated.
- The PAC is then “floated” through the tricuspid valve into the RV and then into the pulmonary artery, using the blood flow to guide the balloon. As the balloon is floated through the different chambers of the heart and into the PA, the waveform trace changes, thus guiding the technician.
- Once in a pulmonary artery the balloon can become “wedged” in the vessel to give a wedge pressure which can approximate LA pressures.
- Once inserted, the balloon is deflated.
Traps of PAC insertion
- Knotting – during insertion, the PAC can loop around itself in the cardiac chambers and even become knotted. One of the key indicators of this is when the PAC has not reached its target location at the expected distance
- NB: RIJ insertion Rule of 10s – 10cm to the RA, 10cms to the RV, 10cms to the PA, 10cms to wedge position
- Arrhythmias – atrial and ventricular arrhythmias may occur. In particular, there is a small risk of RBBB so patients with a LBBB should not have a PAC inserted unless there is immediate access to pacing
- Myocardium/vessel/valve rupture – It is a rare but potentially fatal complication (30-70% mortality). This can occur during catheter insertion or as a delayed consequence if the PAC tip migrates. Ensuring the balloon is adequately inflated (but not overinflated) beyond the catheter tip during insertion reduces risk.
- Pulmonary infarction – can occur if the balloon is left inflated for prolonged periods or from migration of the catheter tip
- Infection – infective endocarditis is a possible risk – ensure sterile insertion technique.
- Thromboembolism or venous air embolism
Deterining Cardiac Output – Thermodilution technique
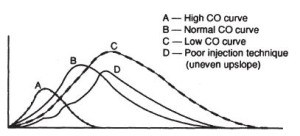
A 5-10ml bolus of injectate e.g. cold 5% dextrose is injected through the proximal injectate port. The distal thermistor measures the change in temperature as the injectate passes through the pulmonary artery. The change in temperature is plotted on an arterial thermodilution curve, as per the Stewart Hamilton Equation:
http://www.creaghbrown.co.uk/anae/hdmon.htm
In normal cardiac output, there should be a rapid increase in temperature followed by a rapid decrease in temperature to normal. In low cardiac output the curve is much wider and flatter. I.e. the rate of blood flow aka cardiac output is inversely proportional to the change in temperature over time. This process is repeated at least 4 times, with the mean of the final 3 measurements taken as the cardiac output.
Measurement Traps
There are a number of reasons why CI may be inaccurate including:
- Catheter misplacement
- Looping/knotting of the PAC
- PAC not in the pulmonary artery
- Thermistor tip is against a wall
- Erratic respiration
- Intracardiac shunt
- Recirculation of injectate to RA/RV – overestimates CO
- Tricuspid regurgitation
- Regurgitation of injectate into RA
- attenuated peak and a prolonged washout phase of the temperature-time curve
- Cardiac arrhythmia
- Inappropriate zeroing of the catheter
- Rapid infusion simultaneously via the IJ line
- Slow injectate delivery
- Inappropriate volume or temperature of injectate
- Too much injectate underestimates CO
- Too little injectate overestimates CO
- Room temp injectate is safer but has less accurate readings
- Cold injectate (0-4 degrees) can temporarily reduce CO and induce bradycardia, but is more accurate
One of the most experienced clinicians, Dr Ray Raper, has been charming the yellow snake for over 35 years. Click here to check out his talk on PA Catheters delivered at SMACC Gold. During this talk, Dr Raper will also discuss the many controversies surrounding PA Catheters and the evidence for and against their use!
Want more??
Check out this talk on insertion of PA catheters and pacing Swan Ganz catheters from Oli Flower (@oliflower) from the Bedside Critical Care conference or this one by Roger Harris (@RogerRdHarris) delivered at SMACC Gold using a pig’s heart for practical demonstration.