Case 19 from Dimity McCracken
[az_accordion_section] [accordion title=”History” id=”acc-1″]
A 47yr old woman presents to the Emergency Dept complaining of severe pain in her right thigh. She says she was bitten by a white-tail spider on the leg about a week ago. When you examine her, she is screaming & writhing about the bed in pain. You notice obvious track marks on her arms & feet. The patient says she used to inject drugs but has been “clean” for over a month. There is a small patch of discoloured skin over her lateral right thigh. A colleague says she presented yesterday with a different story. He is convinced she is drug-seeking. Her obs are as follows:
Sats 98% on room air
RR 32
HR 140
BP 96/51
Temp 38.8*C
What do you do & why?
a) send the patient home
b) observe in ED
c) admit to a general ward under Drug & Alcohol Team
d) order urgent further investigations
[/accordion] [accordion title=”Answer” id=”acc-3″]
You decide to investigate further. Based on her obs, history, examination & risk factors (IVDU) you suspect necrotising fasciitis.
Her ABG shows a marked lactic acidosis with only partial compensation. You give empiric antibiotics & contact the general surgical team immediately. They will be another 20mins finishing up an operation, but ask for a CT in the interim.
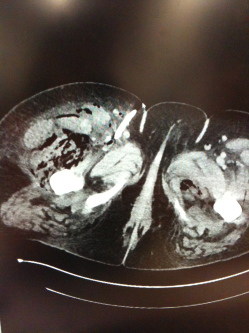
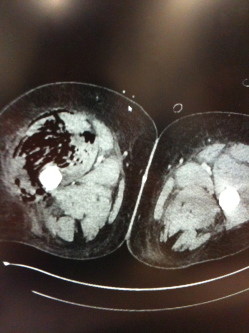
The CT shows large amounts of air throughout the muscle fascia of the right thigh & extends into the pelvic fascia on the left. This is consistent with your suspicions of necrotising fasciitis.
The surgical team arrive & praise you for your rapid referral & antibiotics. The patient is taken to OT for extensive debridements & unfortunately requires a right hind-quarter amputation. After a week in ICU & multiple operations she eventually dies from multiple organ failure.
[/accordion] [accordion title=”Resources” id=”acc-4″]
What is Necrotising Fasciitis (NF)?
NF is an infection of deep tissues that causes progressive destruction of muscle fascia & subcutaneous fat. It spreads along muscle fascia. Initially overlying skin may have little or no visible involvement. This can make diagnosing NF difficult & thus requires a high index of suspicion. There are 2 types of NF, based on microbes found:
Type 1 is polymicrobial usually with at least one anaerobic species, facultative species including Gram-negative rods. Patients are often immunocompromised or have chronic disease processes.
Type 2 is monomicrobial usually Gp A streptococcus, occasionally MRSA or water-bourne species.
While NF can occur in anyone, those with increased risk for developing NF are those with diabetes, immunosuppression, IVDU, alcoholism, chronic liver or renal disease, malignancy, peripheral vascular disease, obesity, skin trauma or recent surgery. NF occurs more commonly on limbs or perineum (Fournier’s Gangrene) but can affect anywhere on the body.
Signs & Symptoms:
– Disproportionately severe pain, however, beware necrotic anaesthesia of skin in later phases.
– Fever, often quite high, & other SIRS response features.
– Skin & overlying soft tissue changes
Initially – very little to see.
Early – cellulitic appearance (erythema, pain, swelling) but with poorly defined margins with oedema extending beyong the margin of erythema. The skin becomes smooth, shiny & tensely swollen
Later – tissues progressively darken with patchy grey discolouration of necrotic skin. Blisters & bullae may develop & the area may look frankly gangrenous. The subcutaneous tissues feel hard & woody. Crepitus can be felt if there is gas present.
Investigations:
– General severe sepsis work-up is warranted, however, surgical exploration is the only definitive way to diagnose NF.
– Cultures (including intra-op) are important. Remind your surgeon that specimens need to be sent fresh, not in formalin!!
– Xray or CT may demonstrate extensive oedema or soft tissue gas, but remember not all NF is caused by gas-forming bacteria.
– Surgical findings include grey necrotic tissues, lack of bleeding, micro-thrombosis of vessels, “dishwater fluid” seeping from tissues, lack of resistance to finger dissection, non-contracting muscle.
Management:
URGENT radical surgical debridement with early empiric antibiotics are the most important aspects of management. NF does NOT improve with antibiotics alone, & delaying surgery beyond 24hrs worsens mortality (http://www.ncbi.nlm.nih.gov/pubmed?term=12925624). Surgery is repeated until the infection is controlled. Thereafter there are daily dressings changes, VAC dressings, skin grafting etc.
Usual severe sepsis cares – resuscitation, early appropriate antibiotics, ICU & organ support all help too. Empirical antibiotics often include: clindamycin plus meropenem, plus vancomycin (if there is a possibility of MRSA) ie. broad spectrum Gram-positive, Gram-negative & anaerobic cover.
Nutritional support is important. There are high protein losses from wounds (often extensive areas involved – think burns). Also, since patients can be going to OT daily, there is frequent inappropriate fasting. Negotiate with anaesthetics for feeds to continue up to (& ideally during) surgery.
The role of hyperbaric O2 is controversial, with no RCT’s in humans.
Down-the-track management of extensive NF becomes similar to that of burns patients.
More out there on the web……..
Radiopaedia on imaging findings in NF: http://radiopaedia.org/articles/necrotising-fasciitis
LifeInTheFastLane’s summary of NF: http://lifeinthefastlane.com/ccc/necrotising-fasciitis/
Another summary of NF, this time from BMJ (not FOAMed, but many hospitals have a subscription – check it out in the library):
http://www.bmj.com/content/345/bmj.e4274
An older, more surgical slant on NF, again from BMJ (be nice to the librarian): http://www.bmj.com/content/330/7495/830
Here is a very useful article on NF, written from a surgical perspective. There is a lot of consideration given to the later stages of wound & pain management. This article is from Current Problems in Surgery & free access to full article via PubMed link below:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4199388/pdf/nihms-622265.pdf
[/accordion] [/az_accordion_section]