So the ED crowd have stolen a march on us following the recent publication of the Sepsis 3.0 Consensus Definitions. And fair play to them for doing so; it has really helped to get the details out in the open.
However, as the Third International Consensus Definitions for Sepsis and Septic Shock was made up of a panel of 19 intensive care physicians (more about this a bit later), it’s only fair that we should take a crack at them too.
Since 1991 we have been defining sepsis using SIRS-based criteria:
- Suspected infection + 2 or more of 4 SIRS criteria = Sepsis
- Sepsis + organ dysfunction = Severe sepsis
- Sepsis + sBP <90mmHg = Septic shock
However, all along there has been an air of disquiet about this SIRS-based model of sepsis. Here are some of the key concerns:
- There is more to sepsis than just inflammation (SIRS is essentially a reflection of inflammation, which may in fact be an adaptive response)
- The inadequate sensitivity and specificity of the SIRS criteria lead to an unhelpful excess of false positives and negatives
- There is an inherent fallacy in the linear progression model of Infection -> Sepsis -> Severe sepsis -> Septic shock
- The definitions were assembled from expert opinion with no quality data to support them
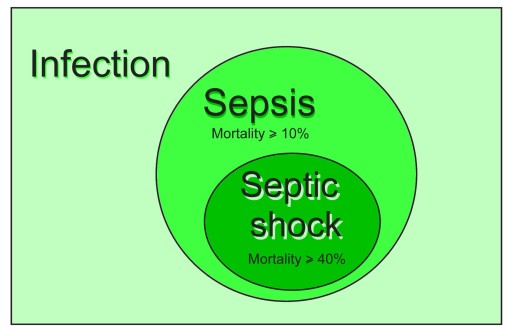
Here are the new definitions as per the Sepsis 3 Consensus update:
“Sepsis is life-threatening organ dysfunction as a result of a dysregulated host response due to known or suspected infection”
“Septic shock is present when there is sepsis with a persistent hypotension requiring vasopressur supprt to maintain a MAP > 65mmHg AND a serum lactate > 2mmol/L DESPITE adequate volume resuscitation.”
As much as possible the committee tried to construct these definitions using available evidence. You can read more about this in the accompanying JAMA articles here:
- Assessment of Clinical Criteria for SepsisFor the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3)
- Developing a New Definition and Assessing New Clinical Criteria for Septic ShockFor the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3)
The new definitions come with some specific criteria.
Sepsis requires a known or suspected infection (easy enough and arguably fairly subjective) with organ dysfunction and an element of life threat. This is where they introduce the use of the SOFA and qSOFA scores.
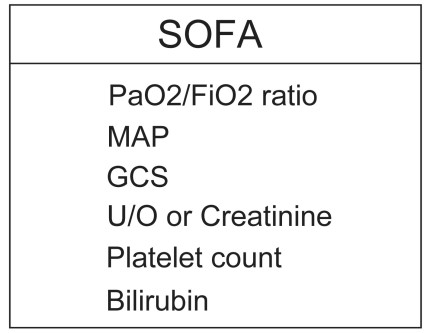
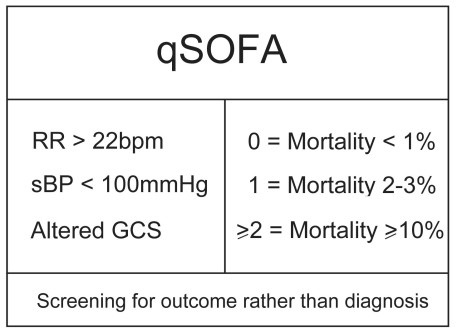
The components of these two scores suggest organ dysfunction and their absolute values indicate the degree of mortality risk.
Here’s how it works.
“I think this patient has an infection. He looks a bit sick, I wonder does he have sepsis, hmm.”
“Well he is tachypnoeic to 28bpm and he’s a bit confused so already his mortality risk in this setting is at lesat 10%.”
“Jeepers, he’s septic. This might kill him. I’d better get cracking, figure out the source, get cultures off and antibiotics in and I think I might give ICU a call.”
So the label “SEPSIS” is not an illness as such. It is a subset risk group of infected patients.
And if this patient is subsequently found to be hypotensive and needing a vasopressor, with a lactate >2mmol/L despite adequate volume resuscitation, then he is in the higher risk group of SEPTIC SHOCK.
And how do I decide whether to use the SOFA score or the qSOFA score? Well I could use either. Realistically, as the SOFA score requires lab results, it can only be calculated once work-up has been started in the ED or is being followed up on the ward or ICU.
The qSOFA only requires three clinical criteria and therefore can be applied by the bedside on the ward, at ED triage or even pre-hospital. Its validity has been derived and tested using a retrospective, large population analysis which you can read in the two papers referenced above. It has yet to be prospectively validated or to be validated outside of North America.
Let’s break this new set of definitions down a bit.
Key features
- Severe sepsis, as a diagnostic entity, no longer exists. It was deemed to add little to the purpose of the new definitions.
- The SIRS-based sepsis definition spectrum is fairly subjective and largely based on expert opinion. The new sepsis and septic shock definitions still have a subjective I think this person has an infection component, while the insertion of the SOFA and qSOFA scores result from a better understanding of sepsis pathophysiology and testing them against a large North American derivation and validation population.
- The new definitions identify a sicker cohort of patients than previously. They (hopefully) exclude the infected who are well and/or likely-to-survive-regardless.
- There is a greater emphasis on life threat and host response dysregulation rather than simple physiological responses that may actually be adaptive (tachycardia, neutrophilia, maybe fever).
Limitations of Sepsis 3.0
- There is no criterion standard test to confirm the diagnosis of sepsis. For the moment, we will still be left with treating the likelihood that this is sepsis, or septic shock, but we may not be able to be definitive. Other systemic illnesses can present with features suggestive of infection and lift SOFA and qSOFA scores by 2 or more points and culture tests may return negative results or the identified infection may be secondary rather than the main driver.
- Sepsis is a non-homogenous amalgamation of triggering infections that set off a dysregulated host response and organ dysfunction. It is not a single disease entity. While the new definitions might make trial results and epidemiology easier to compare, there is still no guarantee that they will be comparing the same thing, depending upon the make up of the triggering illnesses.
- The new sepsis definitions do not really provide a screening tool to diagnose sepsis and septic shock. They are screening tools for the likelihood of a bad (death) outcome in someone with an infection.
- The qSOFA criteria and score were derived by retrospective analysis (associative) of a large dataset (that’s good) of hospitalised patients with presumed infection based on diagnositic coding (selection bias? diagnostic accuracy?). They have not yet been prospectively validated nor tested outside of North America.
- None of this has been tested in a paediatric population and there may be other subgroups missing or under-represented.
- The expert committee who put these definitions together were intensivists from the ESICM and SCCM. No other craft group (ED, pre-hospital, etc) was involved until afterwards when the committee sought peer review.
- Though there has been endorsement of the new definitions by 31 colleges and bodies, not everyone has climbed on board just yet (ACEP, SAEM. There is no reference to Sepsis 3 on the ACEM or CICM websites by the date this article was posted.)
For more picking apart of the Sepsis 3.0 Consensus Definitions, check out these sites:
- Josh Farkas’ PulmCrit – Top ten problems with the new sepsis definition
- Jeremy Faust and Lauren Westafer’s FOAMCast – Sepsis: Redefined
Merits
- 19 intensivists from around the world came to an agreed position on a complex issue and got buy in from 31 peer colleges and bodies. And it only took 18 months from start to finish. Not a bad effort!
- SOFA performs better than the SIRS criteria at predicting mortality risk in ICU populations (AUC 0.74 versus 0.64). That said, it performs no better in non-ICU populations (AUC 0.79 versus 0.76).
- The qSOFA however outperforms both SOFA and SIRS outside the ICU (AUC 0.81). Mind though, this has yet to be prospectively validated.
- The lead authors repeatedly admit that this is an evolving criterion set with scope for modification as better markers and ways to use them are identified and validated.
- One of the biggest benefits has to be that it has multiple groups, colleges and practicioners talking about sepsis and septic shock and this alone will hopefully result in improvements in associated mortality.
Sepsis is not an illness
Sepsis is a risk group of infected patients.
If you want to read more about the new sepsis definitions, including hearing from two of the lead authors, check out the following links:
- The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) (Full text, free)
- Assessment of Clinical Criteria for SepsisFor the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) (Full text, free)
- Developing a New Definition and Assessing New Clinical Criteria for Septic ShockFor the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) (Full text, free)
- Salim Rezaie’s R.E.B.E.L. EM – Sepsis 3.0
- Josh Farkas’ PulmCrit – Top ten problems with the new sepsis definition
- Jeremy Faust and Lauren Westafer’s FOAMCast – Sepsis: Redefined
- Scott Weingart’s EM Crit – Podcast 169: Sepsis 3.0 with Merv Singer
- Scott Weingart’s EM Crit – Podcast 170: Cliff Deutschman with Additional Thoughts on Sepsis 3.0